Diabetes: Risks and Management During Pregnancy: Impact of Gestational Diabetes: Gestational diabetes occurs when the body is unable to produce enough insulin to meet the increased demands of pregnancy, resulting in elevated blood sugar levels. Left unmanaged, this condition can have far-reaching implications for both mother and baby. Some of the potential consequences include:

- Complications During Pregnancy: Gestational diabetes increases the risk of complications such as preeclampsia, premature birth, and cesarean delivery. Expectant mothers may also experience high blood pressure and excessive weight gain.
- Fetal Health Concerns: Elevated blood sugar levels can impact the baby’s growth and development, leading to macrosomia (large birth weight), birth injuries, and respiratory distress syndrome. Babies born to mothers with gestational diabetes may also be at a higher risk of developing type 2 diabetes later in life.
- Long-Term Health Risks: While gestational diabetes typically resolves after childbirth, it can increase the mother’s risk of developing type 2 diabetes in the future. Additionally, children born to mothers with gestational diabetes may have a higher predisposition to obesity and metabolic disorders.

Management Strategies:
Early detection and proactive management are essential in addressing gestational diabetes and minimizing associated risks. Here are some key strategies for managing gestational diabetes during pregnancy:
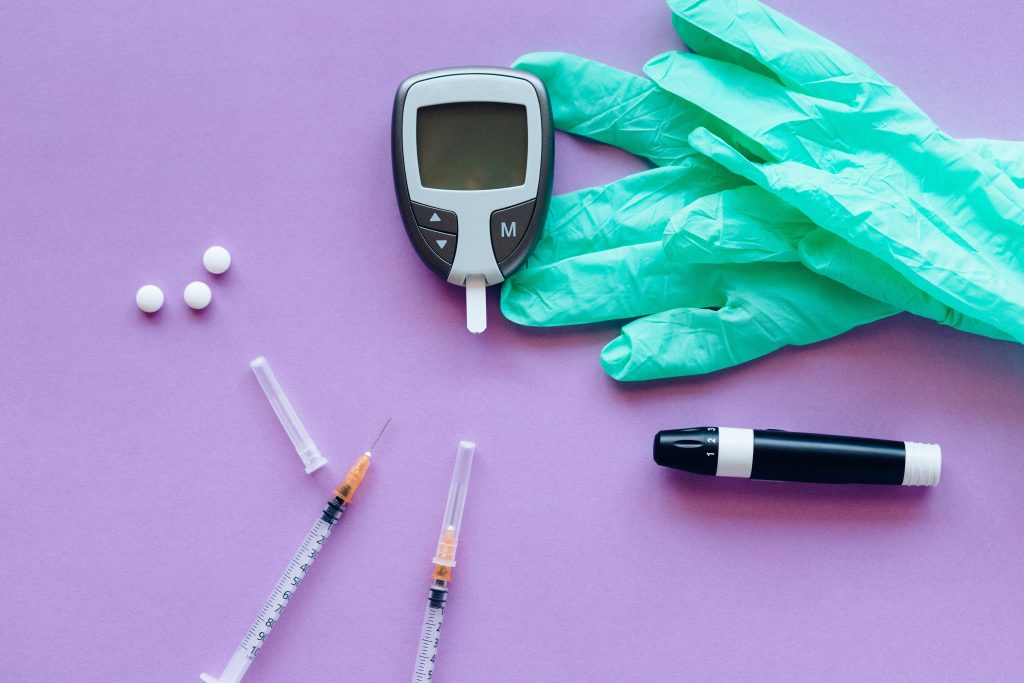
- Regular Blood Sugar Monitoring: Pregnant women with gestational diabetes should monitor their blood sugar levels regularly using a glucometer. Maintaining optimal blood sugar levels through diet, exercise, and medication (if prescribed) is crucial for managing the condition effectively.
- Balanced Diet: A well-balanced diet rich in fiber, lean proteins, and healthy fats can help stabilize blood sugar levels and promote optimal fetal development. Limiting refined carbohydrates and sugary foods is particularly important in managing gestational diabetes.
- Regular Exercise: Physical activity plays a crucial role in managing gestational diabetes by improving insulin sensitivity and promoting healthy weight gain. Low-impact exercises such as walking, swimming, and prenatal yoga are safe and effective options for expectant mothers.
- Medical Monitoring: Pregnant women with gestational diabetes require regular medical monitoring to assess fetal growth, monitor blood sugar levels, and identify any potential complications. Close collaboration with healthcare providers is essential for optimizing maternal and fetal outcomes.
- Postpartum Follow-Up: Following childbirth, women with gestational diabetes should undergo postpartum screening to assess their risk of developing type 2 diabetes. Adopting healthy lifestyle habits, such as maintaining a balanced diet and staying physically active, can help prevent or delay the onset of type 2 diabetes.

In conclusion, gestational diabetes poses significant risks to both maternal and fetal health, emphasizing the importance of early detection and proactive management during pregnancy. By implementing effective strategies for blood sugar control, dietary management, and lifestyle modifications, expectant mothers can minimize the impact of gestational diabetes and promote optimal outcomes for themselves and their babies. Through collaborative care and ongoing support from healthcare providers, women with gestational diabetes can navigate pregnancy safely and ensure the best possible start for their growing families.
