Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age, characterized by irregular periods, excessive androgen levels, and polycystic ovaries. It is often associated with obesity and can significantly impact fertility. In this article, we will delve into the relationship between PCOS, obesity, and infertility, and explore ways to manage these conditions effectively.
PCOS and Obesity
PCOS and obesity are closely intertwined, with each condition exacerbating the other. Obesity is a common feature among women with PCOS, and excess weight can worsen the symptoms of the syndrome. Conversely, PCOS can contribute to weight gain and difficulty in losing weight due to insulin resistance, hormonal imbalances, and metabolic dysfunction.
Insulin resistance, a hallmark of PCOS, leads to elevated insulin levels in the bloodstream, which in turn promotes the storage of fat, especially around the abdomen. This central obesity further exacerbates insulin resistance, creating a vicious cycle that perpetuates weight gain and metabolic disturbances.
Moreover, adipose tissue, or fat cells, produce hormones and cytokines that can disrupt hormonal balance and exacerbate PCOS symptoms. Adipose tissue is also a source of estrogen production, which can further disrupt reproductive hormone levels in women with PCOS.
PCOS and Infertility
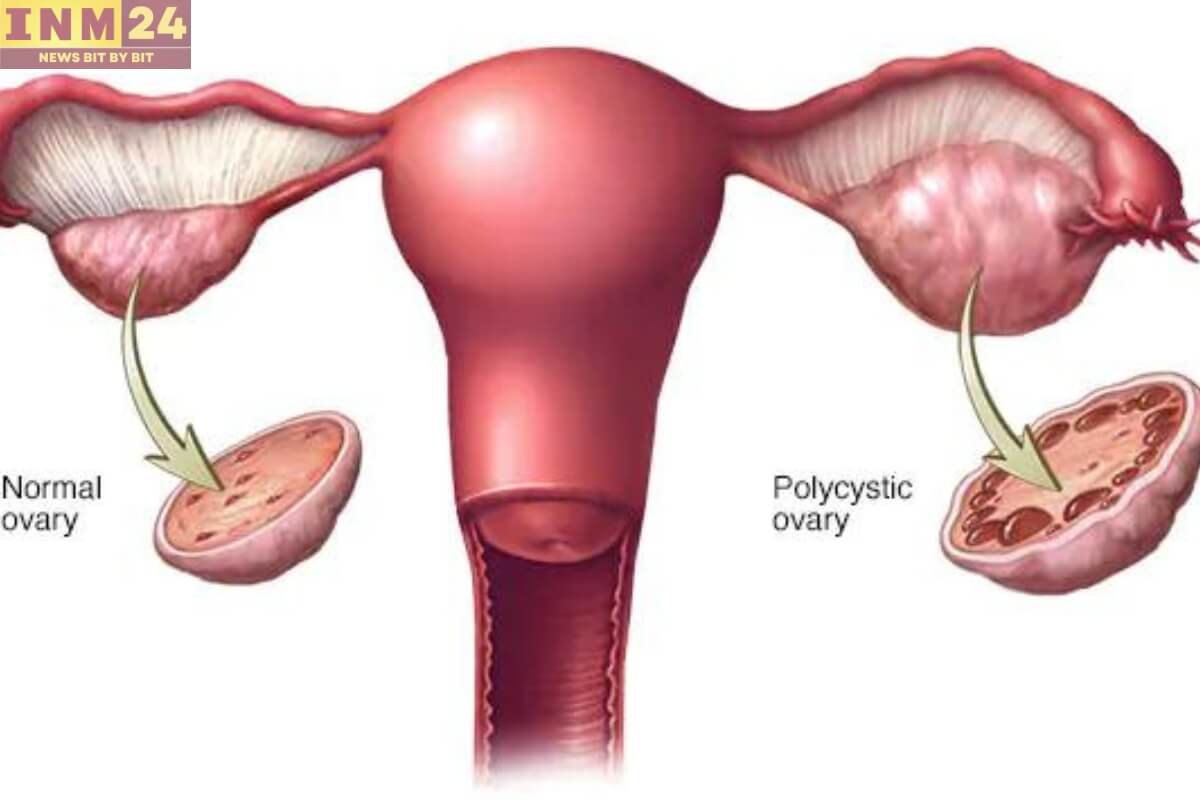
Infertility is a common concern among women with PCOS, primarily due to irregular ovulation or anovulation (lack of ovulation). In PCOS, the hormonal imbalances disrupt the normal menstrual cycle, leading to irregular or absent periods. Without regular ovulation, the release of mature eggs necessary for conception may not occur, making it challenging to achieve pregnancy.
Additionally, high levels of androgens (male hormones) in women with PCOS can interfere with the development and release of eggs from the ovaries. This can result in the formation of follicles that fail to mature and release an egg, further contributing to infertility.
Managing PCOS, Obesity, and Infertility
The management of PCOS, obesity, and infertility often involves a comprehensive approach aimed at addressing underlying hormonal imbalances, managing symptoms, and promoting overall health and well-being.
- Lifestyle Modifications: Adopting a healthy lifestyle, including regular exercise and a balanced diet, is essential for managing both PCOS and obesity. Physical activity helps improve insulin sensitivity, promote weight loss, and regulate menstrual cycles. A diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can help control insulin levels and support weight management.
- Medications: In some cases, medications may be prescribed to help regulate menstrual cycles, reduce androgen levels, and improve fertility. These may include oral contraceptives, anti-androgen medications, and ovulation-inducing drugs such as clomiphene citrate or letrozole.
- Weight Loss: Achieving and maintaining a healthy weight is crucial for managing PCOS and improving fertility outcomes. Even modest weight loss of 5-10% can lead to improvements in insulin sensitivity, menstrual regularity, and ovulation.
- Fertility Treatments: For women with PCOS struggling with infertility, fertility treatments such as ovulation induction with medications, intrauterine insemination (IUI), or in vitro fertilization (IVF) may be recommended to help achieve pregnancy.
- Supportive Therapies: Counseling, support groups, and stress-reduction techniques can help women cope with the emotional challenges of living with PCOS and infertility. Addressing mental health concerns and seeking support from healthcare professionals and peers can be beneficial in managing these conditions.
PCOS, obesity, and infertility are complex and interrelated conditions that require a multidisciplinary approach to management. By addressing underlying hormonal imbalances, adopting healthy lifestyle habits, and seeking appropriate medical care, women with PCOS can effectively manage their symptoms, improve fertility outcomes, and enhance their overall quality of life.